How Could I Help Fund the Baby/ Toddlers Needs After Being Born With Substance Abuse?
The COVID-19 pandemic and the resulting economic recession take negatively affected many people's mental health and created new barriers for people already suffering from mental illness and substance use disorders. During the pandemic, about 4 in 10 adults in the U.S. accept reported symptoms of anxiety or depressive disorder, a share that has been largely consistent, upwards from 1 in 10 adults who reported these symptoms from January to June 2019 (Figure one). A KFF Health Tracking Poll from July 2020 too found that many adults are reporting specific negative impacts on their mental health and well-being, such as difficulty sleeping (36%) or eating (32%), increases in alcohol consumption or substance utilise (12%), and worsening chronic atmospheric condition (12%), due to worry and stress over the coronavirus. Equally the pandemic wears on, ongoing and necessary public wellness measures expose many people to experiencing situations linked to poor mental health outcomes, such as isolation and job loss.
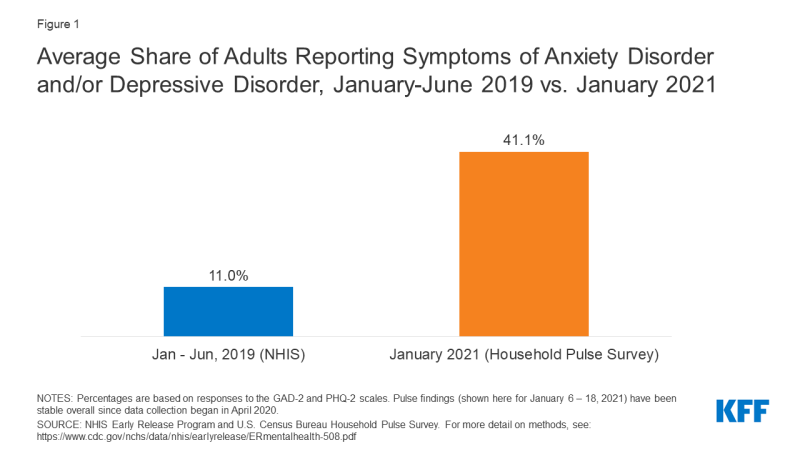
Figure 1: Boilerplate Share of Adults Reporting Symptoms of Anxiety Disorder and/or Depressive Disorder, January-June 2019 vs. January 2021
This brief explores mental health and substance use during, and prior to, the COVID-19 pandemic. Information technology focuses on populations that were particularly at risk for experiencing negative mental health or substance corruption consequences during the pandemic, including young adults, people experiencing task loss, parents and children, communities of color, and essential workers. We draw on KFF analysis of data from the Demography Bureau'due south Household Pulse Survey (an ongoing survey created to capture data on health and economic impacts of the pandemic), KFF Health Tracking Poll data, and data on mental health prior to the COVID-19 pandemic. Central takeaways include:
- Young adults have experienced a number of pandemic-related consequences, such as closures of universities and loss of income, that may contribute to poor mental health. During the pandemic, a larger than average share of young adults (ages xviii-24) study symptoms of anxiety and/or depressive disorder (56%). Compared to all adults, young adults are more likely to report substance utilise (25% vs. 13%) and suicidal thoughts (26% vs. xi%). Prior to the pandemic, young adults were already at high adventure of poor mental health and substance utilise disorder, though many did not receive treatment.
- Research from prior economic downturns shows that chore loss is associated with increased low, anxiety, distress, and low self-esteem and may lead to college rates of substance use disorder and suicide. During the pandemic, adults in households with job loss or lower incomes report higher rates of symptoms of mental affliction than those without job or income loss (53% vs. 32%).
- Inquiry during the pandemic points to concerns around poor mental health and well-existence for children and their parents, particularly mothers, as many are experiencing challenges with school closures and lack of childcare. Women with children are more likely to report symptoms of anxiety and/or depressive disorder than men with children (49% vs. 40%). In general, both prior to, and during, the pandemic, women accept reported higher rates of feet and depression compared to men.
- The pandemic has disproportionately affected the health of communities of color. Non-Hispanic Blackness adults (48%) and Hispanic or Latino adults (46%) are more than likely to study symptoms of anxiety and/or depressive disorder than Non-Hispanic White adults (41%). Historically, these communities of color have faced challenges accessing mental health intendance.
- Many essential workers continue to face a number of challenges, including greater risk of contracting the coronavirus than other workers. Compared to nonessential workers, essential workers are more likely to report symptoms of anxiety or depressive disorder (42% vs. xxx%), starting or increasing substance use (25% vs. eleven%), and suicidal thoughts (22% vs. 8%) during the pandemic.
Both those newly experiencing mental health or substance abuse disorders and those already diagnosed before the pandemic may crave mental wellness and substance use services but could face boosted barriers because of the pandemic.
Prevalence of Mental Illness and Substance Utilise Disorder During the Pandemic
During the COVID-19 pandemic, concerns about mental health and substance apply have grown, including concerns about suicidal ideation. In January 2021, 41% of adults reported symptoms of anxiety and/or depressive disorder (Figure 2), a share that has been largely stable since spring 2020. In a survey from June 2020, 13% of adults reported new or increased substance employ due to coronavirus-related stress, and 11% of adults reported thoughts of suicide in the past 30 days. Suicide rates have long been on the ascension and may worsen due to the pandemic. Early 2020 data bear witness that drug overdose deaths were particularly pronounced from March to May 2020, coinciding with the showtime of pandemic-related lockdowns.
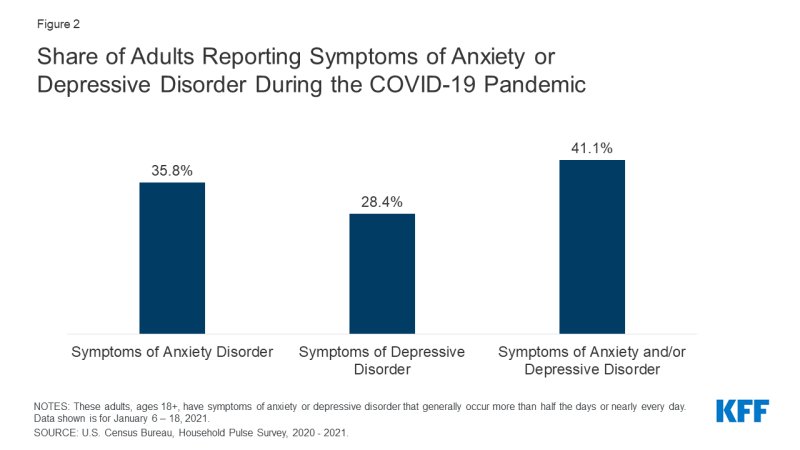
Figure two: Share of Adults Reporting Symptoms of Anxiety or Depressive Disorder During the COVID-19 Pandemic
As was the instance prior to the pandemic, adults in poor general health (which may reflect both physical and mental health) keep to written report higher rates of anxiety and/or depression than adults in good general health.1 , two For people with chronic illness in particular, the already loftier likelihood of having a concurrent mental health disorder may be exacerbated by their vulnerability to severe illness from COVID-19. Recently, a study also found that eighteen% of individuals (including people with and without a past psychiatric diagnosis) who received a COVID-19 diagnosis were later diagnosed with a mental health disorder, such as anxiety or mood disorders. Older adults are too more than vulnerable to severe disease from coronavirus and have experienced increased levels of anxiety and low during the pandemic.
Mental distress during the pandemic is occurring against a properties of high rates of mental illness and substance use that existed prior to the electric current crunch. Prior to the pandemic, one in ten adults reported symptoms of anxiety and/or depressive disorder. Nearly one in v U.S. adults (47 million) reported having whatever mental disease. In 2018, over 48,000 Americans died by suicide,3 and on average across 2017 and 2018, nearly eleven million adults reported having serious thoughts of suicide in the past year. Additionally, deaths due to drug overdose were four times higher in 2018 than in 1999, driven by the opioid crisis.
There are a diversity of ways the pandemic has likely affected mental health, particularly with widespread social isolation resulting from necessary safety measures. A broad body of inquiry links social isolation and loneliness to both poor mental and physical health. The widespread experience of loneliness became a public health concern even before the pandemic, given its association with reduced lifespan and greater risk of both mental and physical illnesses. A KFF Wellness Tracking Poll conducted in late March 2020, shortly later many stay-at-abode orders were issued, found those sheltering-in-place were more likely to report negative mental health effects resulting from worry or stress related to coronavirus compared to those non sheltering-in-place.
Some prior epidemics have induced general stress and led to new mental health and substance employ issues. As the COVID-nineteen pandemic continues, dissimilar populations are at increased risk to feel poor mental wellness and may face challenges accessing needed care.
Immature Adults
Throughout the pandemic, anxiety, depression, sleep disruptions, and thoughts of suicide have increased for many young adults. They have also experienced a number of pandemic-related consequences – such equally closures of universities, transitioning to remote piece of work, and loss of income or employment – that may contribute to poor mental health. KFF analysis of the Household Pulse Survey finds that throughout the pandemic, a large share of immature adults (ages xviii-24) accept reported symptoms of anxiety and/or depressive disorder – 56% as of December 2020 – compared to older adults (Figure 3).
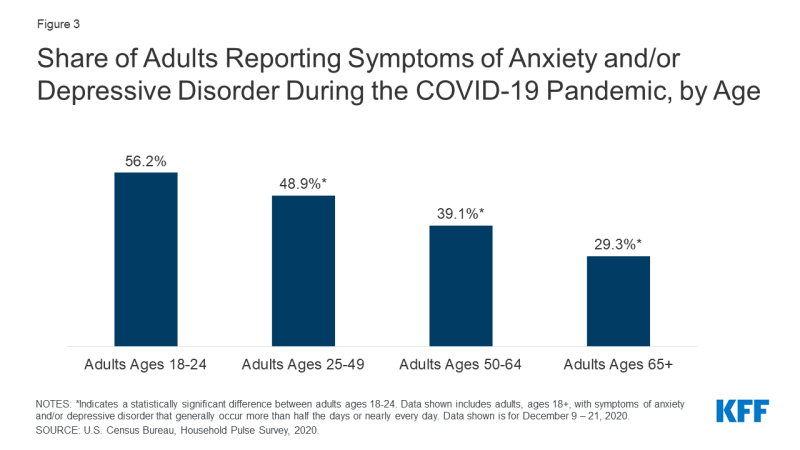
Figure 3: Share of Adults Reporting Symptoms of Anxiety and/or Depressive Disorder During the COVID-19 Pandemic, by Age
An earlier survey from June 2020 showed similar findings for young adults relative to all adults. The survey too institute that substance use and suicidal ideation are especially pronounced for young adults, with 25% reporting they started or increased substance apply during the pandemic (compared to xiii% of all adults), and 26% reporting serious thoughts of suicide (compared to 11% of all adults). Prior to the coronavirus outbreak, immature adults were already at loftier risk of poor mental health and substance use disorder, nonetheless many did not receive handling.
Adults Experiencing Chore Loss or Income Insecurity
Throughout the pandemic, many people across the land have experienced chore or income loss, which has generally afflicted their mental health. Adults experiencing household task loss during the pandemic have consistently reported higher rates of symptoms of anxiety and/or depressive disorder compared to adults not experiencing household job loss (53% vs. 32%, respectively; Figure 4). Similarly, findings from the December KFF Health Tracking Poll testify that households experiencing income or job loss are significantly more likely to report that worry or stress over the coronavirus outbreak has negatively impacted their mental health.
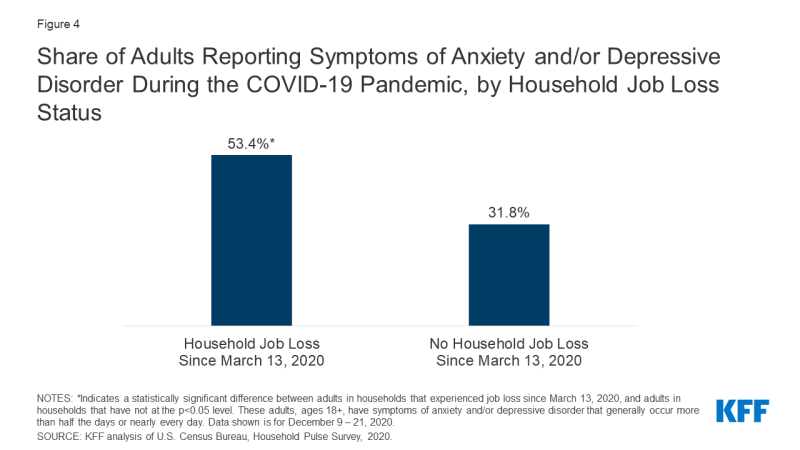
Figure 4: Share of Adults Reporting Symptoms of Anxiety and/or Depressive Disorder During the COVID-19 Pandemic, by Household Task Loss Status
In improver to increased anxiety and low, job loss may lead to other adverse mental health outcomes, such as substance use disorder. During the previous recession, the loftier unemployment charge per unit was besides associated with increases in suicides. A KFF Health Tracking Poll conducted in mid-July 2020 found that, compared to households with no lost income or employment, a higher share of households experiencing income or job loss reported that pandemic-related worry or stress caused them to experience at least ane adverse effect on their mental wellness and well-beingness, such as difficulty sleeping or eating, increases in alcohol consumption or substance utilise, and worsening chronic conditions (46% vs. 59%, respectively).4
KFF Health Tracking Polls conducted during the pandemic accept as well plant that people with lower incomes are more often than not more probable to report major negative mental health impacts from worry or stress over the coronavirus. In Dec 2020, 35% of those earning less than $forty,000 reported experiencing a major negative mental health impact, compared to 21% of those with incomes between $40,000 to $89,999 and 17% of those making $xc,000 or more (Figure 5).
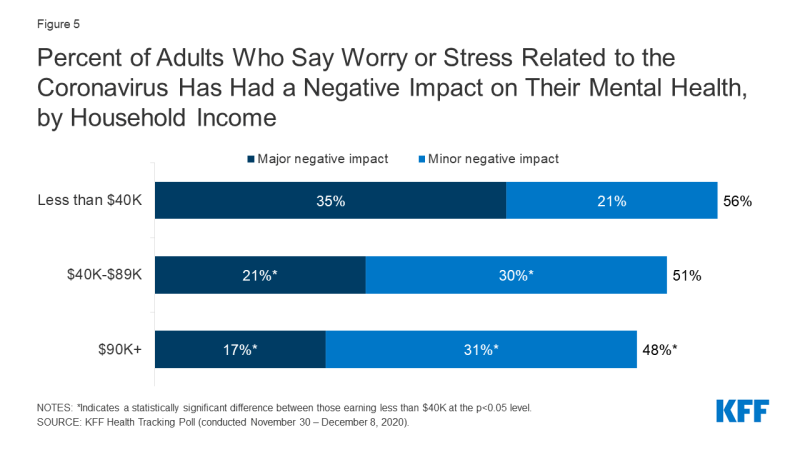
Figure 5: Percent of Adults Who Say Worry or Stress Related to the Coronavirus Has Had a Negative Touch on on Their Mental Health, by Household Income
Parents and Children
To assistance dull the spread of coronavirus, many schools and childcare centers across the U.Due south. have closed and transitioned to virtual instruction for at to the lowest degree some time. With these closures, children and their parents are experiencing ongoing disruption and changes to their daily routines. Enquiry during the pandemic highlights concerns effectually poor mental health and well-beingness for children and their parents. For example, many parents with school-anile children are now more concerned most their children's emotional well-being than prior to the pandemic. Both parents and their children take experienced worsening mental wellness since the first of the pandemic, and women with children are more than probable than their male counterparts to study worsening mental health.
Throughout the pandemic, we detect that adults in households with children under the historic period of 18, compared to adults in households without, are slightly more likely to written report symptoms of feet and/or depressive disorder (45% vs. 41%, respectively, every bit of Dec 2020).v Specifically, among households with children under the age of 18, women have been more likely than men to report symptoms of anxiety and/or depressive disorder throughout the pandemic (equally of December 2020, 49% vs. 40%, respectively; Figure 6). Similarly, KFF Health Tracking Polls conducted during the pandemic have by and large found that among parents, women are more probable than men to written report negative mental health impacts.6
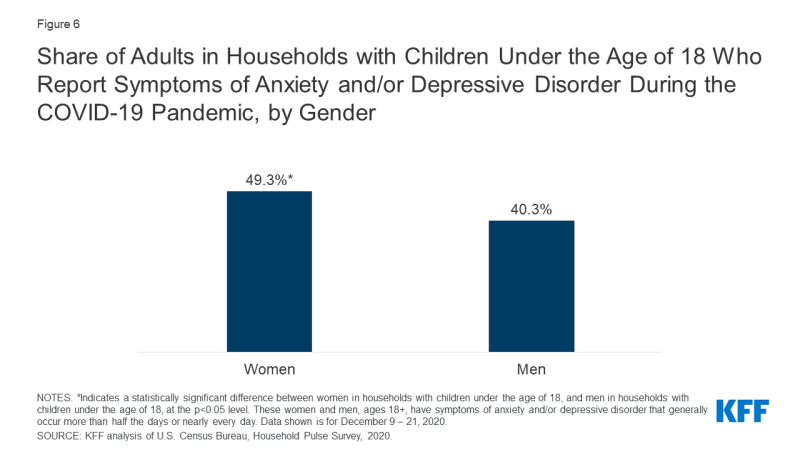
Effigy 6: Share of Adults in Households with Children Under the Historic period of eighteen Who Report Symptoms of Anxiety and/or Depressive Disorder During the COVID-nineteen Pandemic, by Gender
Throughout the pandemic, women have been more likely to report poor mental health compared to men. For example, 47% of women reported symptoms of feet and/or depressive disorder compared to 38% of men in December 2020. Amidst women in the workplace, more than 1 in four are because leaving their jobs or reducing their hours, with many citing burnout and household responsibilities as the primary reason. Even earlier the pandemic, women were more likely than men to report mental health disorders, including serious mental affliction.
Existing mental illness amongst adolescents may be exacerbated by the pandemic, and with many schoolhouse closures, they do non accept the same access to key mental health services. Prior to the pandemic, more than than one in ten (16%) adolescents ages 12 to 17 had anxiety and/or depression.7 Children may experience mental distress during the pandemic due to disruption in routines, loss of social contact, or stress in the household. Additionally, child abuse may be increasing during the pandemic. Child abuse-related emergency department (ED) visits dropped during the COVID-19 outbreak; however, the severity of injuries amidst child corruption-related ED visits has increased and resulted in more than hospitalizations. Child abuse tin can lead to immediate emotional and psychological problems and is too an adverse babyhood experience (ACE) linked to possible mental illness and substance misuse later in life. Educators play a critical role in the identification and reporting of child corruption. However, with school closures and stay-at-dwelling house orders, information technology is probable that many cases are going undetected, and that at-risk children accept increased exposure at abode to their abusers.
Substance apply is also a business organisation amid adolescents. Prior to the pandemic, xv% of high school students reported using an illicit drug, and 14% reported misusing prescription opioids. Lone substance use (as opposed to social employ) has increased among adolescents during the pandemic, which is associated with poorer mental health. Suicidal ideation is yet some other major concern for adolescents during the pandemic. While suicide was the tenth leading cause of deaths overall in the U.S. earlier the pandemic, it was the second leading cause of deaths among adolescents ages 12 to 17.eight Prior to the pandemic, suicide rates were peculiarly pronounced amongst Blackness and LGBTQ youth.
Communities of Color
The pandemic'due south mental wellness bear upon has been pronounced amidst the communities of color also experiencing unduly loftier rates of COVID-19 cases and deaths. Black and Hispanic adults take been more likely than White adults to report symptoms of anxiety and/or depressive disorder during the pandemic (Figure vii). This disparate mental health touch comes in addition to Blackness and Hispanic communities experiencing disproportionately high rates of coronavirus cases and deaths (overall as well as amongst health intendance workers and in nursing homes), and negative fiscal impacts. Additionally, Black parents more frequently than White parents have reported negative impacts of the pandemic on their children's education, their ability to treat their children, and their relationships with family members. Prior to the pandemic, Blackness and Hispanic people were less likely to receive needed behavioral health services compared to the general population. Additionally, deaths by suicide – which may increase due to the pandemic – have historically been much higher than average amid Native American communities.
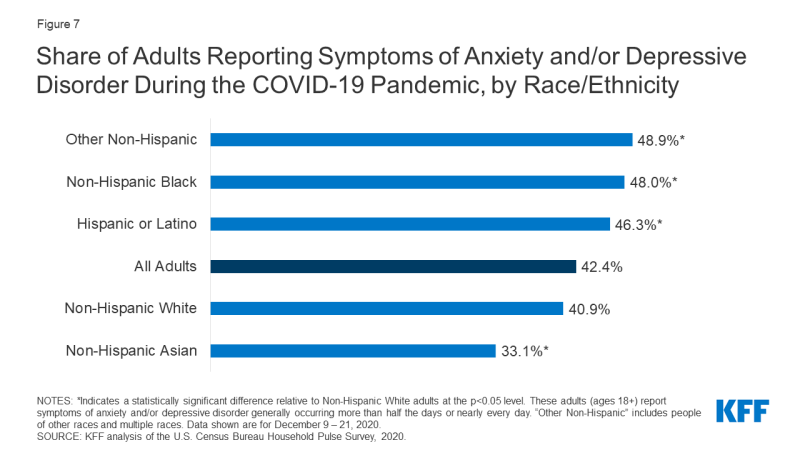
Figure 7: Share of Adults Reporting Symptoms of Anxiety and/or Depressive Disorder During the COVID-19 Pandemic, by Race/Ethnicity
Essential Workers
Essential workers during the COVID-19 pandemic, such as health intendance providers, grocery store employees, and mail and packet delivery personnel, have shown high rates of poor mental wellness outcomes. These workers are by and large required to piece of work outside of their dwelling and may be unable to practice social distancing. Consequently, they are at increased take chances of contracting coronavirus and exposing other members of their household. A KFF analysis found that essential workers face up additional challenges, including difficulties affording basic necessities as a result of the pandemic. These factors may contribute to poor mental wellness outcomes for these workers. Every bit shown in Figure viii, essential workers are more probable than nonessential workers to written report symptoms of anxiety or depressive disorder (42% vs. xxx%, respectively), starting or increasing substance utilize (25% vs. eleven%), or because suicide in the past 30 days (22% vs. viii%).
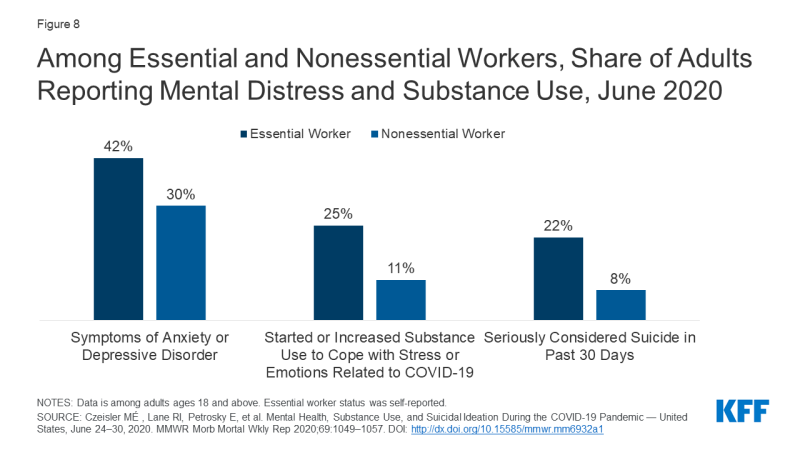
Figure 8: Among Essential and Nonessential Workers, Share of Adults Reporting Mental Distress and Substance Use, June 2020
During the pandemic, frontline health care workers have reported feelings of feet and depression and thoughts of suicide. The KFF Health Tracking Poll conducted in mid-April 2020 plant that 64% of households with a wellness intendance worker said worry and stress over the coronavirus caused them to experience at least one adverse impact on their mental health and well-beingness, such as difficulty sleeping or eating, increases in alcohol consumption or substance employ, and worsening chronic conditions, compared to 56% of all households. Prior to the pandemic, nurses and physicians were already prone to experiencing exhaustion, with physicians likewise having an elevated risk of suicide.
Policy Responses and Considerations
Throughout the pandemic, leading public health organizations — including the CDC, SAMHSA, the World Wellness Organization, and the United nations — have released general considerations and resources addressing the mental health and well-being of both full general populations and specific, loftier-risk groups during the pandemic. In the U.Southward., some steps accept been taken at both the federal and state levels to address the pandemic's impact on mental wellness, just with mental wellness problems on the ascension, key problems are probable to persist.
Congress has addressed some of the acute demand for mental health and substance use services through 2 stimulus bills enacted during the pandemic. The Consolidated Appropriations Act, which was signed into police in December 2020, includes about $4.25 billion in funding for mental health and substance use services. It besides builds on existing legislative efforts to boost insurer compliance with federal mental health parity rules. The Coronavirus Aid, Relief, and Economical Security Act (CARES Human activity), a stimulus bill passed in March 2020, as well allocated funding for mental wellness and substance use services, including a $425 million appropriation for apply by SAMHSA, in addition to several provisions aimed at expanding coverage for, and availability of, telehealth and other remote intendance for those covered past Medicare, individual insurance, and other federally-funded programs. It likewise allowed for the Department of Veterans Affairs to arrange expansion of mental wellness services to isolated veterans via telehealth or other remote care services. Other efforts to accost mental health needs include substantial increases in the employ of telehealth for mental wellness services, aided early on past the federal regime and many states expanding coverage and relaxing regulations for telehealth services. Looking ahead, the Biden administration and Congress could take additional steps to accost mental wellness and substance use bug, including administrative actions addressing suicide amongst LGBTQ youth, mental health parity, the opioid crisis, veteran mental wellness services, and school-based mental health services.
Given the pandemic's implications for both people with new or pre-pandemic mental health conditions, the crisis spotlights new and existing barriers to accessing mental health and substance utilise disorder services. Among adults reporting symptoms of anxiety and/or depressive disorder, more than than 20% report needing but not receiving counseling or therapy in the by calendar month during the pandemic. Limited access to mental health care and substance utilise treatment is in part due to a current shortage of mental health professionals, which has been exacerbated by the pandemic. The pre-pandemic shortage of psychiatric hospital beds has also worsened with the surge of COVID-19 patients needing beds at hospitals across the nation.
Admission to mental health and substance use care was a concern prior to the pandemic. In 2018, among the vi.5 million nonelderly adults experiencing serious psychological distress, 44% reported seeing a mental health professional in the past year. Compared to adults without serious psychological distress, adults with serious psychological distress were more likely to exist uninsured (20% vs 13%) and exist unable to beget mental health intendance or counseling (21% vs iii%).9 For people with insurance coverage, an increasingly common barrier to accessing mental wellness care is a lack of in-network options for mental health and substance use care. Those who are uninsured already face paying total price for these and other health services. Every bit unemployment continues to affect millions of people, who in turn may lose task-based coverage, some may regain coverage through options such as Medicaid, COBRA, or the ACA Market, but others may remain uninsured. With an unprecedented share of people reporting symptoms of anxiety or depressive disorder, the potential consequence of California v. Texas (a example challenging the constitutionality of the entire ACA) is important to consider. Prior to the ACA, people with a preexisting condition similar depression might have been denied health coverage or charged higher premiums, and many individual market place plans did not embrace any mental health or substance use services.
Looking Ahead
The pandemic has both curt- and long-term implications for mental health and substance use, specially for groups at risk of new or exacerbated mental health disorders and those facing barriers to accessing intendance. Phased COVID-19 vaccinations are taking place across the country, perhaps signaling that the end of the pandemic is on the horizon. Notwithstanding, many of the stressful conditions employed to mitigate the spread of the coronavirus are likely to persist for the near future, given the slow and troubled rollout of vaccinations across the country, instances of people refusing the vaccine due to fear or uncertainty, and the need for vaccinated people to go along taking existing precautions to mitigate the outbreak.
History has shown that the mental health bear upon of disasters outlasts the physical affect, suggesting today'due south elevated mental health need will go along well beyond the coronavirus outbreak itself. For example, an analysis of the psychological toll on health care providers during outbreaks found that psychological distress can last upwardly to 3 years subsequently an outbreak. Due to the fiscal crisis accompanying the pandemic, there are too meaning implications for mortality due to "deaths of despair." A May 2020 analysis projects that, based on the economic downturn and social isolation, additional deaths due to suicide and booze or drug misuse may occur by 2029.
As policymakers continue to discuss farther actions to convalesce the burdens of the COVID-xix pandemic, it volition be of import to consider how the increased need for mental health and substance employ services will likely persist long term, fifty-fifty if new cases and deaths due to the novel coronavirus subside.
This work was supported in part by Well Being Trust. We value our funders. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
Source: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
0 Response to "How Could I Help Fund the Baby/ Toddlers Needs After Being Born With Substance Abuse?"
Kommentar veröffentlichen